The Basics
Surgery & Surgical Menopause for PMDD/PME
Surgery is the last line in treatment for premenstrual disorders reserved for those who have not gained relief through other evidence-based treatments. Surgery involves removal of the ovaries and often uterus, which induces menopause and is called surgical menopause. On this page we cover the basics on surgery for PMDD/PME and also surgical menopause.
Why do people have surgery for PMDD/PME?
What does the surgery do and how does it work for PMDD/PME?
What Is The Correct Surgery For PMDD?
What are the symptoms of surgical menopause?
Which Surgeries Result in Surgical Menopause?
How is surgical menopause different from the natural menopause?
For more in-depth information and answers to commonly asked questions you can visit our searchable FAQ.
Why do people have surgery for PMDD/PME?
Surgery for a premenstrual disorder is a big decision with life-long impacts on the body. Removing your ovaries is an invasive procedure that immediately causes surgical menopause and menopause symptoms. The decision to have surgery is not made lightly. However, when someone with PMDD/PME has ruled out all other evidence-based treatments, and still suffers severe symptoms that keep them from functioning in their normal life, surgery can be a life-changing, effective treatment.
“SSRIs worked quite well for me in my 20s and made my symptoms pretty manageable for a long time. However, in my 30s my symptoms severely worsened and despite working my way through the available treatment options, nothing worked (and often made me feel worse). It took me a while to get my head around the fact that surgery could be an option - I read lots of blogs and joined groups. At the end of the day, I felt like I was out of options and wanted my life back.” - Patient
Essentially, surgery for a premenstrual disorder is the last treatment option when your symptoms are severe, and no other interventions have worked.
Having surgery at a younger age for severe PMDD? Listen to this podcast where IAPMD Volunteers, Rachel & Anna, share their experiences of having surgery in their early 20’s:
What does surgery do and how does it work for PMDD/PME?
While many people refer to surgery for PMDD/PME as a ‘hysterectomy’ (removal of the uterus) - the essential part of the procedure is actually the removal of both ovaries (bilateral oophorectomy - or bilateral salpingo oophorectomy if the fallopian tubes are also removed). PMDD is a severe negative reaction in the brain to the natural rise and fall of estrogen and progesterone, triggered by ovulation, a process that takes place in the ovaries. By removing the ovaries (when all other forms of cycle suppression have not worked) you remove ovulation and thus, remove those fluctuations from happening.
Pre - surgery (fluctuations)
At a basic level - PMDD is caused by a sensitivity in the brain to the natural hormone fluctuations that occur as part of the menstrual cycle. The brain has a negative reaction to those ups and downs of the sex hormones.
Post - surgery (steady levels of hormones)
By removing the ovaries, and therefore removing ovulation/the menstrual cycle, and using estrogen therapy (HRT) to keep the hormone levels even and steady, you eliminate the fluctuations that trigger PMDD symptoms.
To learn more about the different types of surgery for PMDD/PME, visit considering surgery.
What Is The Correct Surgery For PMDD?
When discussing surgery for PMDD, you will often hear people talking about having a ‘hysterectomy’ which can cause lots of confusion and misunderstanding. When surgical menopause is used as a final treatment for Premenstrual Dysphoric Disorder (PMDD), the removal of the ovaries is actually the critical part of treatment since the ovaries cause hormone fluctuations, and therefore trigger PMDD. The surgical removal of both ovaries is called a ‘Bilateral Oophorectomy.’
After removal of the ovaries, estrogen hormone replacement therapy (HRT) is used to reduce menopausal symptoms and bone and heart risks. Estrogen used alone can cause a buildup of the uterine lining, leading to hyperplasia, so a form of progesterone is often used as well to prevent this. However, since many individuals with PMDD have a sensitivity to progesterone (which can trigger PMDD-like symptoms), progesterone ‘add-back’ is not the preferred route. In many cases, the uterus is removed (a hysterectomy) in addition to the ovaries.
When progesterone is well tolerated by the individual, the uterus can sometimes be kept, and combined HRT is used (i.e., estrogen and progesterone together).
Patient tolerates progestogen-based treatments
If you tolerate progestogen-based treatments, then you may only need a Bilateral Oophorectomy. This is the removal of both the ovaries. Your surgeon may also suggest BSO (Bilateral Salpingo - Oophorectomy) which means your fallopian tubes are removed as well.
Your uterus and cervix can remain in place (so no hysterectomy is needed, just ovary removal) and the progestin add-back HRT can be given in the form of the Mirena IUS or combined HRT (such as Tibolone) to protect from hyperplasia (monitoring is required).
Learn more about progestogen addback here.
Patient does not tolerate progestin-based treatments
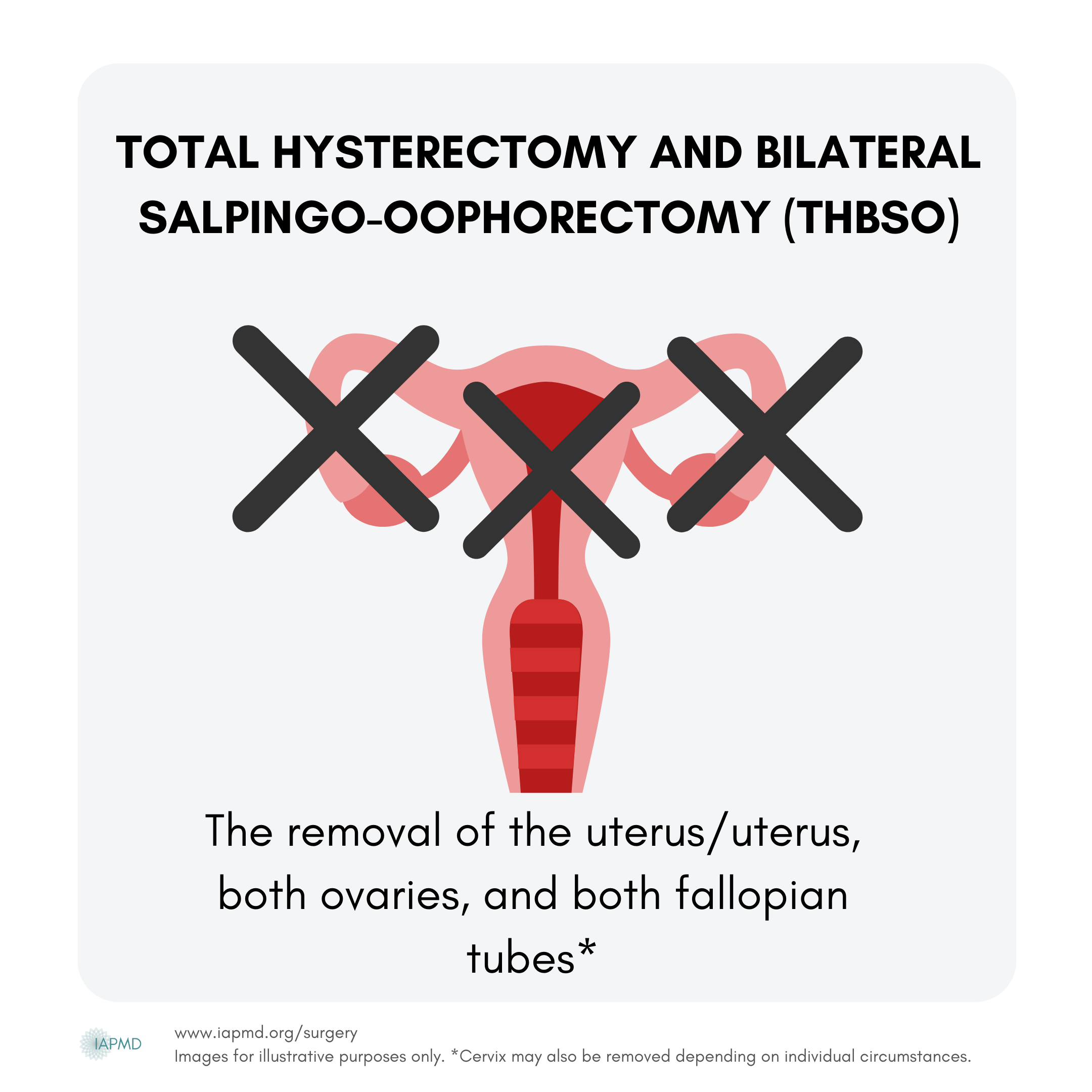
If you do not tolerate progestogen-based treatments then you would need a Total Hysterectomy with Bilateral Oophorectomy (THBO). This is the removal of the uterus/womb, cervix and both ovaries. Your surgeon may also suggest to remove your fallopian tubes as well.
This means that you can use estrogen-only HRT and do not need to use progesterone add-back.
This is known as estrogen therapy (ET) - you can learn more here.
If you are unsure if you are progesterone intolerant, you can read more here.
A hysterectomy without ovary removal is not a treatment for PMDD.
Some surgeons will remove only the ovaries in special circumstances where physical risks are abnormally high due to other medical conditions; however, this is not standard practice for the treatment of PMDD.
What is Surgical Menopause?
Surgical menopause (sometimes called ‘surmeno’) is a surgically-induced menopause that refers to the menopausal (low) hormone state that occurs following surgical removal of both ovaries. This procedure is called a bilateral oophorectomy and is the last line treatment for PMDD/PME, when less invasive treatments have not been effective. When both ovaries are removed, this removes the main source of estrogen, progesterone, and testosterone in your body. This means you will no longer have a menstrual cycle and you are in surgical menopause.
Removal of just one ovary (leaving the other) is called a unilateral oophorectomy. When just one ovary is removed, this does not result in surgical menopause and the remaining ovary continues to produce normal hormone cycling each month.
Often for treatment of a premenstrual disorder, (though not always), a surgical removal of the uterus (a hysterectomy) is performed at the same time as removal of your ovaries (oophorectomy) due to an intolerance to progestogen add-back. If you have a hysterectomy but keep your ovaries, you will not experience a surgical menopause - your hormones will continue to cycle as they normally would each month, even though your uterus is gone (and you will have no menstrual bleeding). A hysterectomy without ovary removal is not a treatment for PMDD.
What are the symptoms of surgical menopause?
Symptoms of surgical menopause are caused by estrogen deficiency. Following the surgical removal of the ovaries, you become post-menopausal immediately. As your hormone levels drop you may experience a sudden onset of menopausal symptoms. These may be mild, moderate, or severe, depending on your particular situation. These symptoms can be minimized by taking Hormone Replacement Therapy (HRT), or alternatives (see estrogen alternatives here) if hormones are not an option following surgery.
Symptoms include, but are not limited to:
Vasomotor symptoms (e.g., hot flushes and sweats)
Musculoskeletal symptoms (e.g., joint and muscle pain)
Effects on mood or anxiety (e.g., feeling abnormally sad or worried)
Urogenital symptoms (e.g., vaginal dryness, needing to urinate frequently)
Sexual difficulties (e.g., low sexual desire, painful sex).
Other - headaches, sleep issues, skin changes
Menopausal symptoms, as a result of estrogen deficiency, can also be long-term - but individual experiences vary. HRT can reduce these symptoms and can be safely taken long-term, except in some circumstances.
Long-term Health Risks
The ultra-low levels of estrogen in surgical menopause can cause bothersome menopausal symptoms, but more importantly, they can reduce the length and quality of your lifespan by increasing risk for various health conditions. We will address each below.
For those under the age of 40 who enter surgical menopause, using HRT (Hormone Replacement Therapy) can reduce or eliminate the serious long-term health risks associated with surgical menopause, including:
osteoporosis and broken bones
cardiovascular disease (e.g., heart attack, stroke)
dementia and Parkinson’s disease
psychiatric disorders (e.g., mood or anxiety disorders)
vulvar and vaginal atrophy
sleep disorders (e.g., persistent and impairing insomnia)
higher risk of death by any cause
To summarize, surgical menopause is known to cause all of the above symptoms and health risks-- but these problems can generally be reduced or eliminated by using estrogen therapy following surgery through to the typical age of menopause (51 years). Most individuals in surgical menopause choose to continue some level of estrogen through at least age 60 to maintain symptom relief.
Which Surgeries Result in Surgical Menopause?
The following surgical procedures will result in surgical menopause:
*The cervix may also be removed depending on individuals reaction to HRT in both THBO and THBSO surgeries.
** A radical hysterectomy is typically performed when someone has cancer of the cervix, ovaries, fallopian tubes, or uterus. It is not a standard treatment for PMDD/PME.
How is surgical menopause different from natural menopause?
Natural menopause occurs after a transition period (which can last from months to years) called perimenopause where the body gradually makes less estrogen to a point where the ovaries stop releasing eggs (menopause). Surgical menopause occurs instantly when you have both ovaries surgically removed.
Risks can be reduced by using transdermal estrogen (gels/patches which are absorbed through the skin)
Natural menopause
A natural menopause occurs when the ovaries stop releasing eggs and, as a result, the levels of sex steroid hormones (estrogen, progesterone, and testosterone) fall. The average age of natural menopause is 51 years of age, but any time after 45 is considered ‘normal.’ The years during the menopausal transition are called perimenopause, which can last months or even up to years. Periods often become heavier and more sporadic during this time, and menopausal symptoms (e.g., night sweats, hot flashes, or vaginal dryness) begin to appear. If you are going through menopause naturally, you will be considered postmenopausal a year to the day of your last period. If menopause occurs between the ages of 40 and 45, this is referred to as early menopause. One in a hundred women will experience menopause under the age of 40 – this is referred to as premature menopause or premature ovarian insufficiency (POI).
Surgical menopause
In those who undergo a bilateral oophorectomy (removal of both ovaries), the transition into menopause is immediate and known as surgical menopause. The symptoms can be sudden and may be more intense than those experienced in natural menopause, especially in younger individuals.
Following surgery to remove your ovaries, you will become postmenopausal instantly.
Sudden symptoms of menopause often occur quickly following surgery, and can be unpleasant or distressing, so it is important to work with an experienced healthcare professional to look after both your short-term and long-term health during this rapid transition.
There is so much to learn when it comes to PMDs and surgery - check out our searchable knowledge base which is packed full of evidence-based answers for commonly asked questions. From considering surgery, right though to thriving in Surgical Menopause, this is your go-to source!
This project was financially assisted by The Patty Brisben Foundation for Women’s Sexual Health. The views expressed herein do not necessarily represent those of The Patty Brisben Foundation for Women's Sexual Health.